Breast Augmentation
Conveniently located to serve the areas of Beverly Hills and Los Angeles, CA

Dr. Kenneth Hughes, Harvard-trained, board certified plastic surgeon, has performed thousands of breast augmentations in Los Angeles and Beverly Hills throughout his career, and he offers patients from all over the world the ability to choose among the many options in breast augmentation based upon patient anatomy and goals.
There are two forms of breast augmentation currently available – 1) breast augmentation with saline, silicone, or gummy bear implants and 2) breast fat grafting or breast fat transfer.
This procedure page describes breast augmentation with breast implants. Dr. Kenneth Hughes also has a procedure page for breast augmentation with breast fat transfer or breast fat grafting.
Contents
- 1 Before and After Photos
- 2 About Breast Augmentation
- 3 Top Rated Doctor
- 4 Breast Evaluation
- 5 Incisions
- 6 IMF (inframammary) Incisions
- 7 Periareolar Incision
- 8 Saline Transumbilical Breast Implants
- 9 Transaxillary
- 10 Types of Breast Implants
- 11 Ideal Implant Profile
- 12 Breast Implant Volume
- 13 Mini Breast Augmentation
- 14 Cost
- 15 What to Expect
- 16 Breast Implant Videos
- 17 Recovery
- 18 Breast Augmentation Articles
- 19 Schedule Today
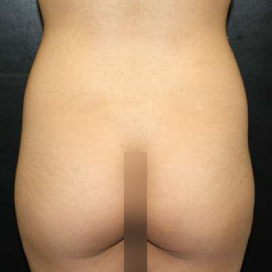
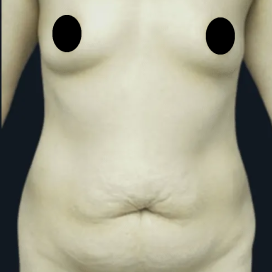
Before and After Photos
About Breast Augmentation
Dr. Hughes has performed breast augmentation both above the muscle (subglandular) and under the muscle (submuscular), and he offers saline and silicone implants in a broad array of types and profiles.
If you have a particular way you would like your breast augmentation performed, Dr. Kenneth Hughes has done it for other patients.
Dr. Hughes also performs a number of other breast procedures, including the breast lift, breast augmentation with fat grafting, and breast reduction.
Transgender Breast Augmentation Surgery for MTF (Male to Female) Patients
Dr. Kenneth Hughes performs breast augmentation surgery for those transgender patients who are transitioning from male to female. The breast augmentation surgery can be performed with fat transfer or breast implants. The breast implant surgery is by far the more common, as breast fat transfer surgery can only increase the cup size by 3/4 cup.
Top Rated Doctor
Breast Evaluation
During the consultation, Dr. Kenneth Hughes in Los Angeles will discuss your unique anatomical details, and he will suggest an approach and an implant for you. If you are confused or undecided on breast augmentation, Dr. Kenneth Hughes will make everything about your surgery clear and formulate a plan just for you.
In order to help choose the best breast implants for a patient, Dr. Kenneth Hughes will evaluate the patient’s chest wall and breast form. He will point out chest wall asymmetry or deformity as well as breast asymmetry or deformity and nipple areola complex (NAC) asymmetry as well as NAC deformity. Chest wall issues cannot be changed, and Dr. Hughes will advise the patient on what breast issues can be affected for the better.
He will also comment on relative level of breast droop or ptosis, and he will advise the patient as to whether a breast lift is necessary and the type of breast lift needed.
In many cases, a breast lift and breast implants can be combined to improve fullness of the breasts and lift the breasts at the same time. This allows for fuller and perkier breasts that do not droop. When a patient desires a reduction in droop without an increase in fullness, it is best to choose a breast lift without implants. Many patients who have breast augmentation and breast lift may be interested in other procedures as well including mommy makeover, tummy tuck, liposuction, and Brazilian buttlift. Frequently, Dr. Kenneth Hughes performs these combination procedures to produce a fabulous overall body rejuvenation that requires only one recovery period.
Dr. Kenneth Hughes will point out if the skin envelope is loose and whether or not stretchmarks are present. Stretchmarks frequently remain the same or become worse with breast augmentation. Very few breast augmentation patients have enough breast tissue to permit a subglandular augmentation. Most patients with small breasts or hypomastia are better served by a submuscular augmentation to permit a more natural breast takeoff and better camouflage for the implant.
Dr. Kenneth Hughes will determine your preference for saline, silicone, or gummy bear implants. He will inform you of the positives and negatives of each so that you can make an informed decision about the type of implant. Dr. Hughes will explain the differences in as much detail as you wish.
It is important that patients have realistic expectations for this procedure. Viewing breast augmentation before and after photos is an excellent way to visualize your potential results.
Incisions
Dr. Kenneth Hughes in Los Angeles can perform breast augmentation or breast enhancement with any available breast implant through any incision.
Dr. Kenneth Hughes performs breast augmentation through the belly button (transumbilical augmentation, TUBA). This approach allows breast augmentation to be performed without any scars on the breast. The scar is hidden inside the belly button. Few people have the training to perform this type of breast augmentation, and that is the primary reason why many surgeons perform augmentation through other incisions.
Dr. Kenneth Hughes also performs breast augmentation through the armpit (transaxillary). This incision also allows for placement of implants without any scars placed on the breast. The scar is placed in the natural underarm crease, making it virtually undetectable.
Dr. Kenneth Hughes also performs breast enlargement through the most common incisions made under the areola (infraareolar or periareolar) or in the fold of the breast (inframammary fold). Whatever you as the patient want, Dr. Hughes can deliver.
IMF (inframammary) Incisions
The inframammary breast augmentation places the incision underneath the breast within the breast fold. This is the most common approach to breast enlargement, because it is technically the easiest method to perform. The incision is made, the inferior border of the pectoralis major muscle is identified, and the pocket is dissected.
It may be necessary to use this incision for larger implants or gummy bear implants, which are more difficult to deform due to its higher molecular cohesion. Saline or silicone implants can be placed through this incision.
Periareolar Incision
The periareolar breast augmentation involves making an incision under the areola and dissecting through the breast to reach the pectoralis muscle. The periareolar breast augmentation may be performed for women who may not have a well defined inframammary fold or who are not good candidates for the transumbilical or the transaxillary approaches. The areolar size must be large enough to allow placement. This may be a limiting factor in women with smaller areolae who want larger silicone or gummy bear implants.
The incision generally heals well as it is placed in a natural pigment transition zone. A property executed periareolar breast augmentation should have no impact on breast feeding or lactation as the ducts should not be disturbed. The plane of dissection runs parallel to the ducts and not perpendicular.
Sensation is always a concern with any form of breast augmentation. The incision may compromise small portion of the cutaneous sensitivity to the areola and nipple. In addition, the rates of infection and capsular contracture may be higher for this approach due to the proximity to the bacteria present in and below the nipple areolar complex.
Once again, this all comes down to weighing the risks and benefits for each individual and Dr. Hughes is an expert at helping you understand all of these elements.
Saline Transumbilical Breast Implants
The transumbilical breast augmentation places an incision in the hood of the belly button (umbilicus) and creates a tunnel to the breast. The great thing about this approach is the no one will know you had this done as the scar is nearly imperceptible. Despite the naysayers, this technique allows for very precise pocket dissection with a true breast augmentation expert like Dr. Kenneth Hughes.
Most surgeons have never been trained nor have they performed this method and have no expertise or knowledge with regard to the procedure. Dr. Hughes offers all alternatives to breast augmentation so that each patient can have what each patient wants. This method has an extremely low rate of hematoma and infection. This method can be used for saline breast implants but not for silicone implants.
Transaxillary
The transaxillary breast augmentation places the breast implant by making an incision in the armpit (axilla). From this point a tunnel is created underneath the pectoralis major muscle and the implant is inserted through this tunnel.
This procedure can be performed bluntly or under direct or endoscopic visualization. Both saline and silicone implants can be placed through this method. The rates of infection and capsular contracture may be higher for this method due to bacterial translocation from incision.
Types of Breast Implants
Breast implants typically consist of saline, silicone, and gummy bear implants. Saline implants consist of a silicone shell into which a saline solution (salt water solution) is placed or filled. Silicone implants consist of a silicone shell and a prefabricated silicone matrix. Silicone breast implants largely fall into two groups: cohesive gel and gummy bear implants (which are solid in their truest sense).
In general, silicone implants are more expensive than saline implants. Silicone implants require MRIs to monitor for rupture. They feel more natural and show less rippling through the skin. The rippling is frequently only observed after years of having implants, as the implants thin the breast and subcutaneous tissue.
Conversely, saline implants are cheaper. If the saline implants rupture, the body will absorb the saline and the deflation will become evident to the patient.
Different companies make different types of gummy bear implants with varying amounts of silicone crosslinking or cohesivity so it can be confusing. Dr. Hughes in Los Angeles prefers Mentor silicone cohesive gel implants to minimize rippling and maintain softness.
The form stable implants or gummy bear implants are indeed harder as the silicone becomes more and more solid. Dr. Hughes has used Allergan and Sientra as well and thinks all companies make reasonable implants.
Smooth or Textured Breast Implants?
Dr. Kenneth Hughes in Los Angeles usually places smooth implants and does not routinely place textured implants, as they offer no advantages and may have a risk that is higher for implant related breast cancer. Textured implants were originally developed to reduce the rate of capsular contracture in above the muscle (subglandular) breast implant augmentation.
There are almost no indications to performing this subglandular procedure but may include animation deformity correction and professional athlete muscle performance concerns following submuscular implant augmentation.
Round or Teardrop (Anatomic) Breast Implants?
In almost all women, round implants will produce a better result as the mass of most breast tissue is located in the inferior aspect of the breast. Thus, round implants give more upper pole fullness, which is usually lacking due to involution or lack of development.
Teardrop or anatomic implants were developed for women after mastectomy to approximate the shape of breast if starting with nothing. Thus, if used in most women, the result is a more matronly look with less upper pole fullness.
Ideal Implant Profile
This factor actually has very little to do with the result. Almost no low profile implant is ever utilized. Almost all implants placed are moderate, moderate plus, or high(full) profile. Very few ultra high profile breast implants are used as they may have a higher probability of thinning tissue over time.
The difference in diameter and implant height among moderate, moderate plus, and high(or full) profile implants is very little and may be less than a centimeter in diameter for a given volume. Dr. Hughes will help you determine what profile may be best for your chest wall and breast imprint measurements once a volume is selected.
Breast Implant Volume
While large breast implants make sense for certain patients, others may benefit more from small breast implants. Dr. Hughes in Los Angeles can assess very quickly what range of volumes would be reasonable based upon patient breast width compared to implant diameter for given profiles.
Dr. Hughes can offer a relatively narrow range of volumes to produce the best fit for an individual. In addition, looking at the various implants and trying them on in the office can help allay some of the patient trepidation associated with this decision.
Mini Breast Augmentation
Many patients find a mini breast augmentation to be their ideal option. This variation on the standard technique involves smaller implants (typically smaller than 275 cc); standard breast augmentation usually features implants that are between 275 cc and 400 cc in volume.
The smaller size of the implants used in a mini breast augmentation allows the doctor to create a smaller incision for insertion during the surgery. Because the incisions are smaller, the procedure is less invasive and results in a smaller degree of post-surgical bruising and swelling. The recovery time is also shorter.
These implants are ideal for achieving a subtler and more natural aesthetic change. The mini breast augmentation is best for patients with a smaller frame and less breast tissue, as it lowers the chance of implant rippling and other potential issues.
Cost
- Breast implant surgery costs $9500 for saline breast implants.
- Breast implant surgery costs $10,500 for silicone breast implants.
- Breast implant surgery costs $12, 500 for gummy bear implants.
Please note that pricing and cost for breast augmentation may vary based on the individual needs of the patient. Dr. Kenneth Hughes operates in Los Angeles and Beverly Hills so the breast augmentation surgery cost may vary based upon location as well.
What to Expect
Dr. Hughes frequently sees patients for 1) initial consultation and 2) preoperative appointment and finally 3) on the surgery day to address any additional questions or concerns.
The anesthesiologist will discuss with the patient the type of anesthesia administered, which is usually general anesthesia so that the patient is comfortable and completely unaware. The patient is taken to the operating room, wherein an IV is started and the patient is put to sleep. The procedure takes about 30 minutes to 1 hour to perform.
Patients typically remain in recovery for 1 to 2 hours and then depart for home or the hotel. Patients are asked to get all of their prescriptions filled well in advance of surgery so that pain medications, nausea medications, and antibiotics will be available upon departing from the surgery center. Dr. Hughes does not recommend a surgical bra as this can irritate incisions.
Breast Implant Videos
Recovery
Dr. Hughes typically sees patients within the first few days to a week following surgery. The patient usually has 2 to 3 days of pain during which the patient takes pain pills to provide relief. Thereafter, most patients do not need the narcotics.
Patients can return to work within 1 to 3 days or whenever they feel is appropriate.Dr. Hughes recommends no breast massage and does not want patients to exercise for 4 weeks after surgery. Some patients may find that the implants are in perfect position almost immediately or the implants may take a few weeks to settle.
Dr. Hughes recommends not wearing a bra after surgery until Dr. Hughes tells you to do so. The bra can irritate or possibly open the incisions.
Potential complications of breast enlargement surgery include hematoma, seroma, wound infection, alterations in nipple sensation. (In Dr. Kenneth Hughes’s extensive experience, these represent less than 1% of cases).
Implant complications include displacement, rippling, and rupture. Implant rupture occurs at a rate of 1% per implant per year.
Dr. Hughes has a strong understanding of the ways to prevent these potential complications and can effectively address them if they happen to occur.
Breast Augmentation Articles
The History of Breast Augmentation in the US
The Evolution of Saline and Textured Implants
Silicone Implants and Implant Controversies
Evaluation of the Breast Augmentation Surgery Patient
Determining Implant Size and Incisions in Breast Augmentation: Inframammary and Infraareolar
Incisions and Approaches to Breast Augmentation: Transaxillary and Transumbilical
Capsular Contracture in Breast Augmentation
Complications of Breast Augmentation
Schedule Today
Breast augmentation is a popular procedure that can deliver impressive results. To find out more about breast augmentation in Los Angeles, schedule a consultation with Dr. Kenneth Hughes by contacting our office.